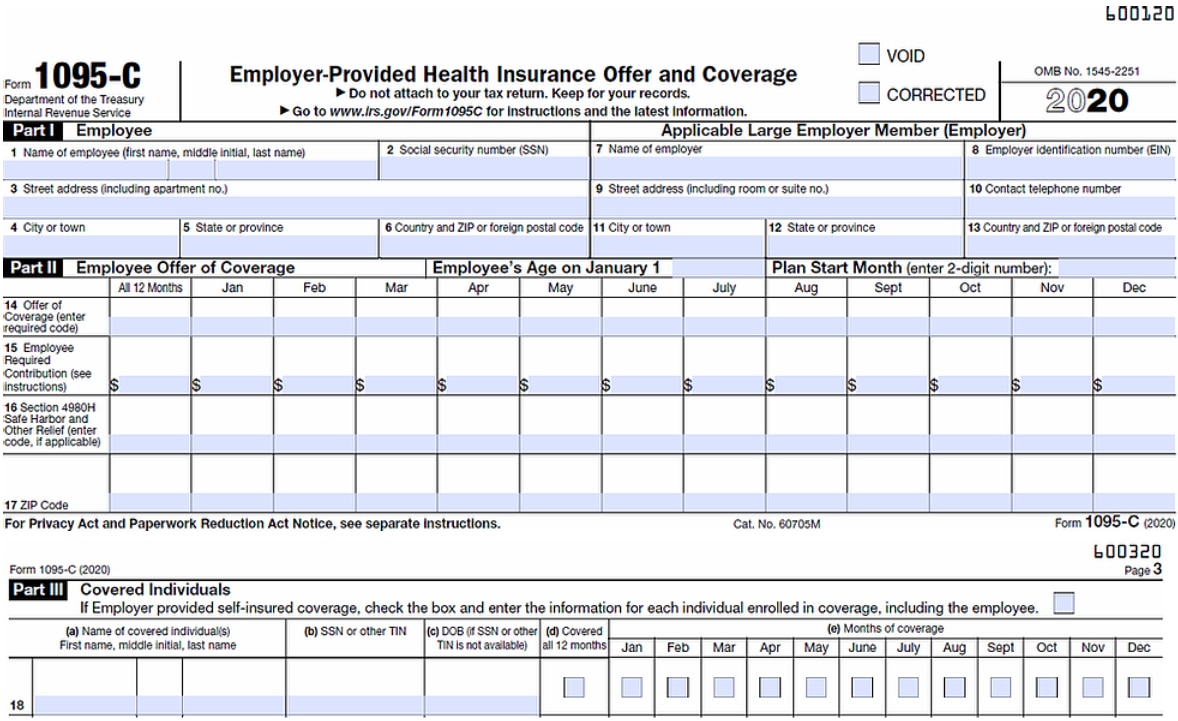
Applicable Large Employers (for example, you left employment with one Applicable Large Employer and began a new position of employment with another Applicable Large Employer) In that situation, each Form 1095C would have information only about the health insurance coverage offered to you by the employer identified on the formDec 30, 15 · For example, if an employer intends to file a separate Form 1094C for each of its two divisions to transmit Forms 1095C for each division's fulltime employees, one of the Forms 1094C filed must be designated as the Authoritative Transmittal and report aggregate employerlevel data for both divisions, as required in Parts II, III, and IVMay 21, 21 · There are six different scenarios for claiming a Limited NonAssessment Period when filing annual Forms 1095C with the IRS Firstyear as ALE period January through March of the first calendar year in which an employer is an ALE, but only for an employee who was not offered health coverage by the employer at any point during the prior
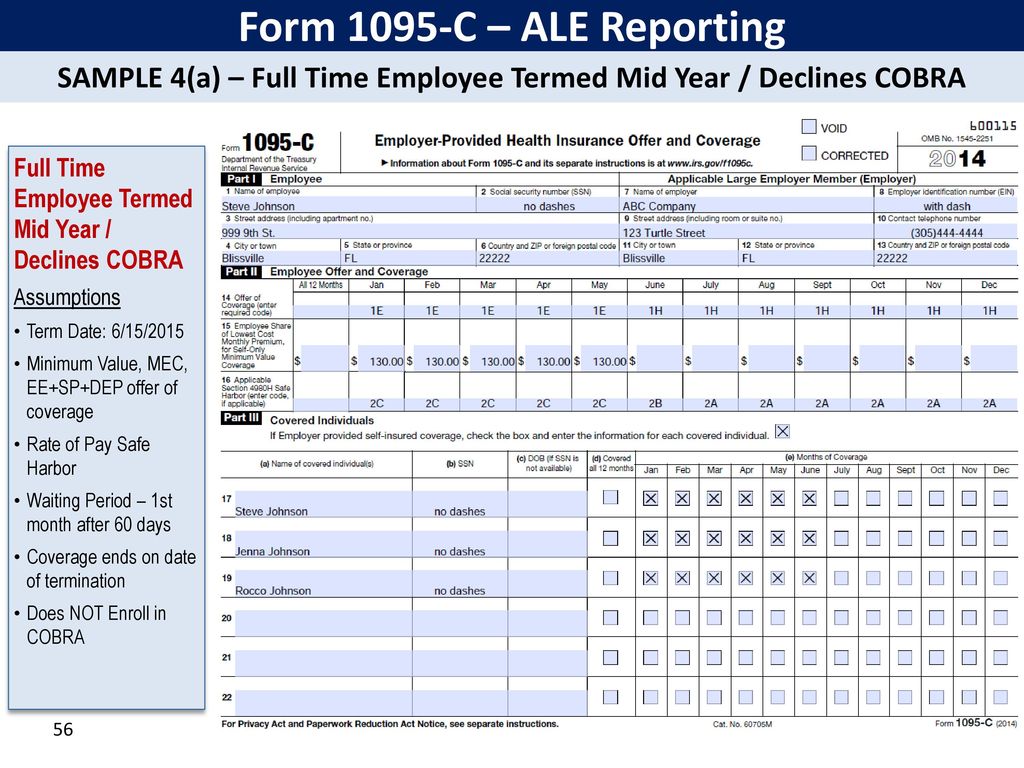
Irs Affordable Care Act Reporting Forms 1094 Ppt Download
How to complete 1095 c
How to complete 1095 c-Nov 21, 19 · You do not have to complete a Form 1095C for an employee who was in a limited nonassessment period for all months of employment during a calendar year For example, if you use a 12month initial measurement period and an employee was hired on March 1, 18, you would not need to complete a 18 Form 1095C for that employeeLet's Look At The Most Common 1095C Coverage Scenarios



Irs Form 1095 C Codes Explained Integrity Data
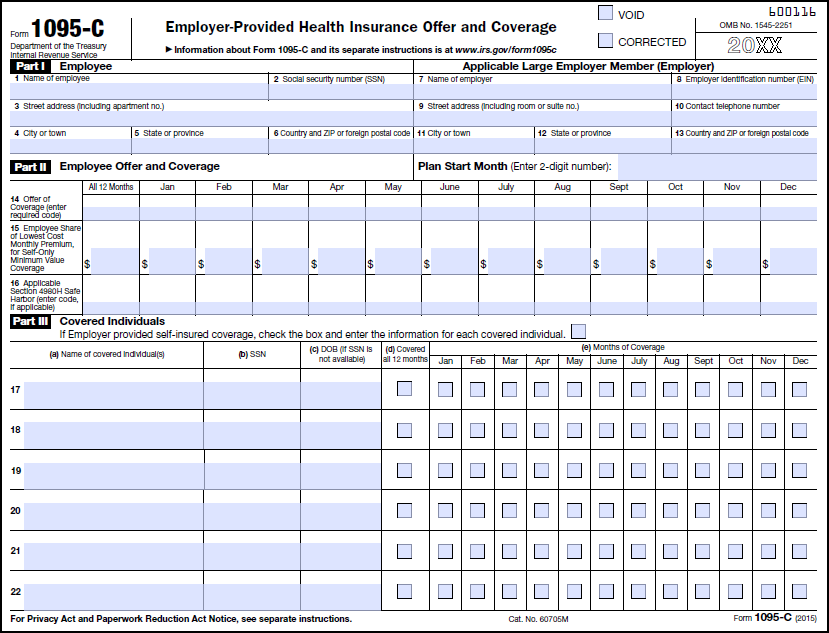
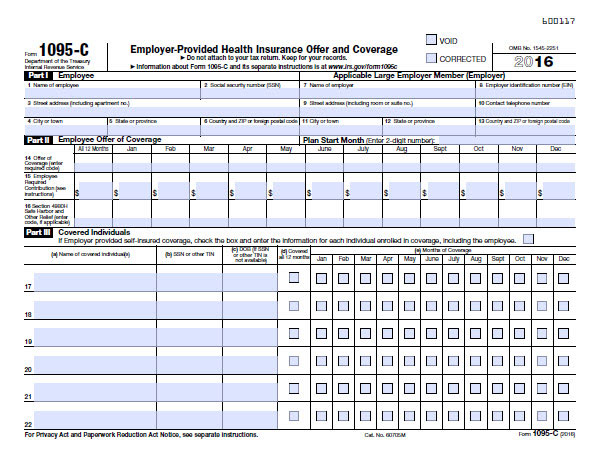
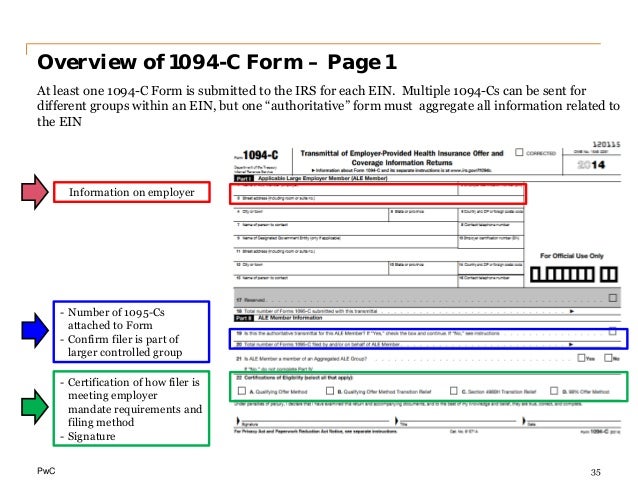
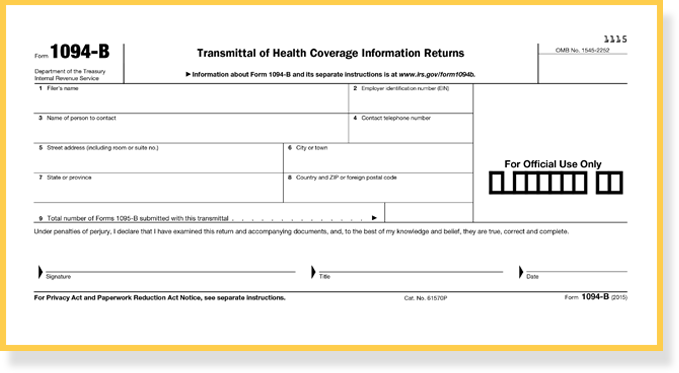
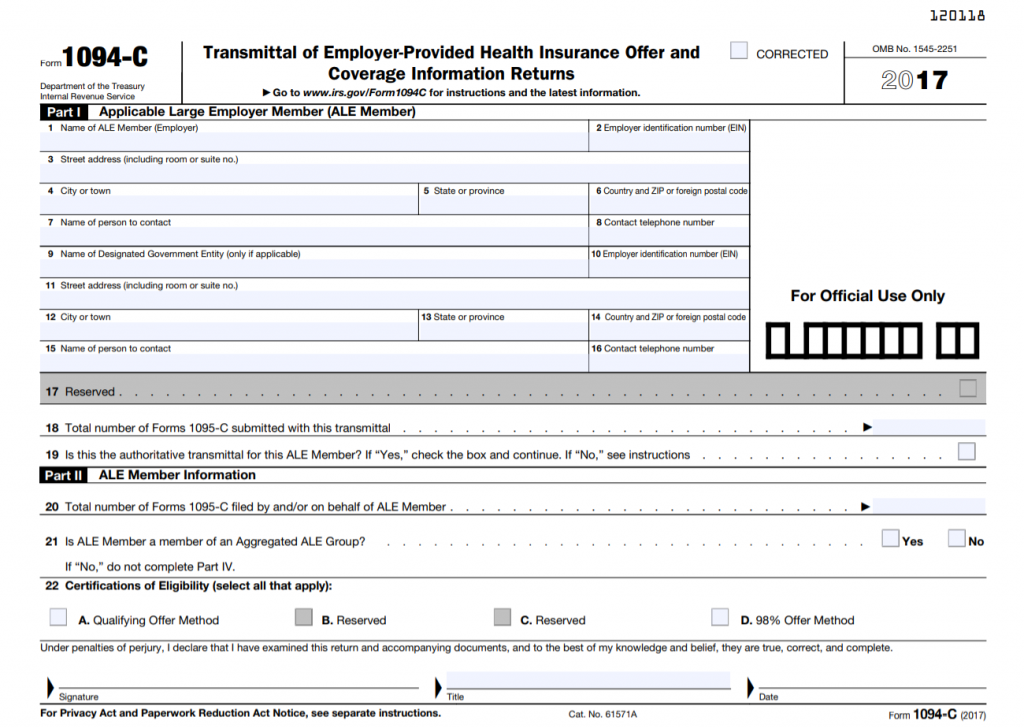
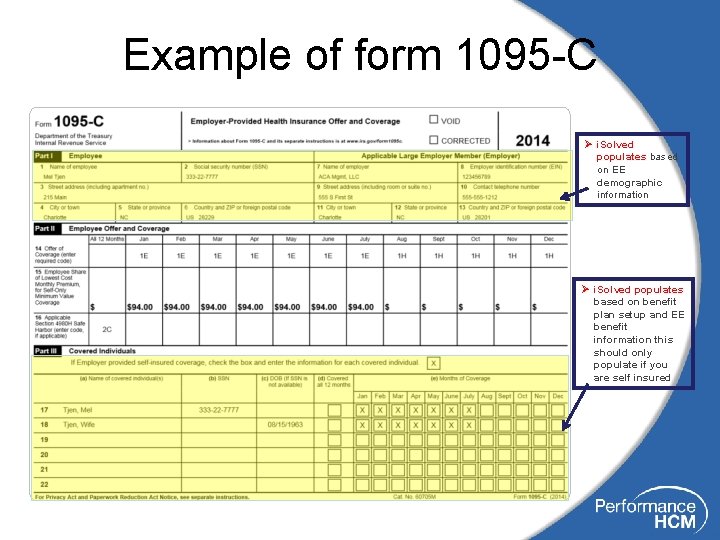
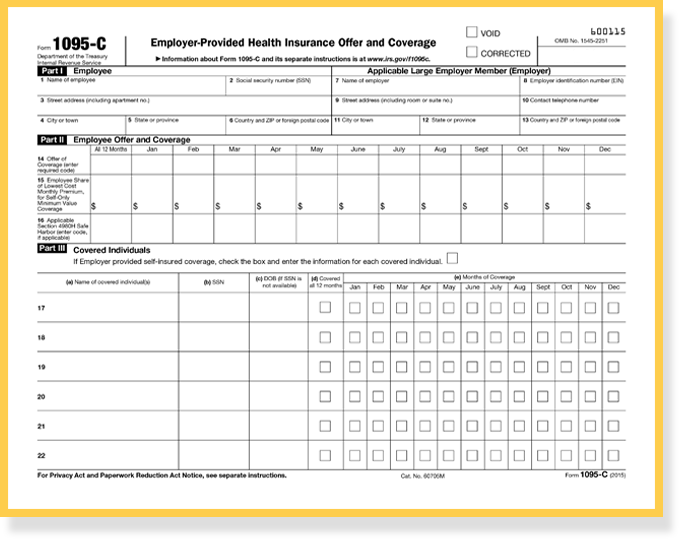
Dec 15, 15 · Line 18 Total number of Forms 1095C (those going to employees) associated with this form Remember, the address on this form must be the same as the Forms 1095C associated with this form Line 19 Confirm whether this is the authoritative transmittal If yes, you'll need to complete parts II, III and IV, to the extent applicableNov 01, 19 · For example, selfinsured small employers must complete and file Forms 1095B and 1094B (the transmittal form) with the IRS, as well as provide fulltime employees with a copy of Form 1095B Small employers also are required to file Forms 1095C and 1094C if they are members of a controlled or affiliated service group that collectively hasHow to complete Form 1095C In order to stay compliant with the Affordable Care Act in 16, companies with a fulltime staff of 50 or more will need to file a Form 1095C for each employee We'll help you figure out how it works
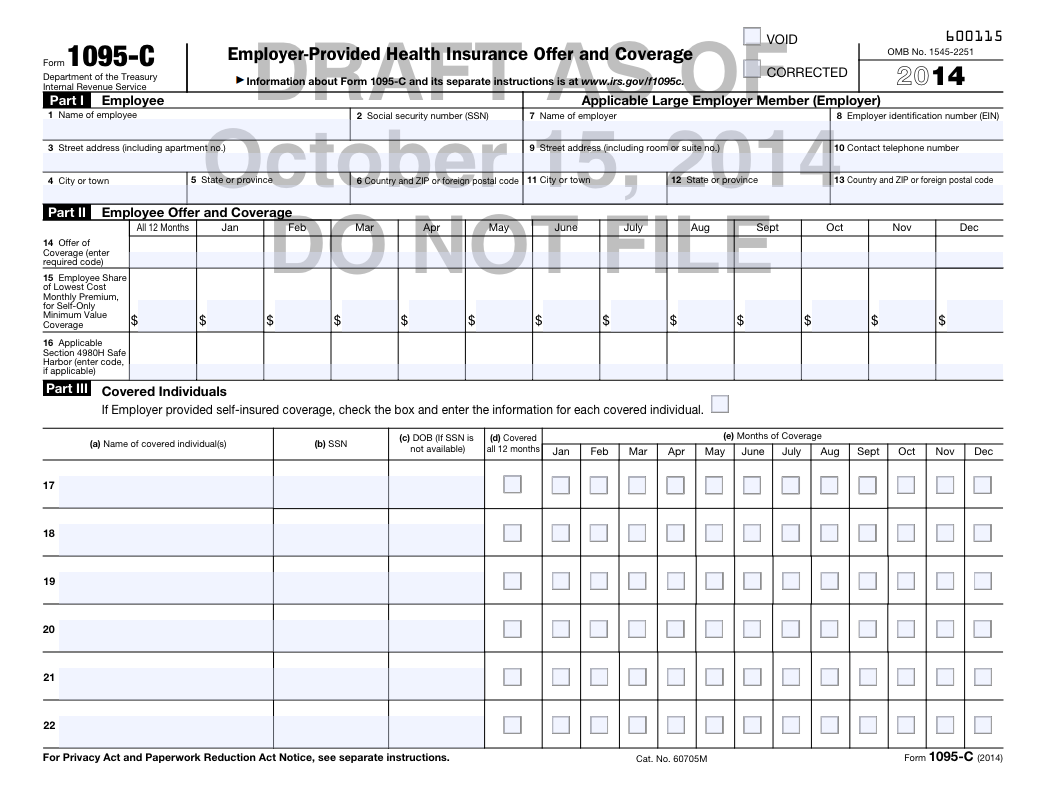
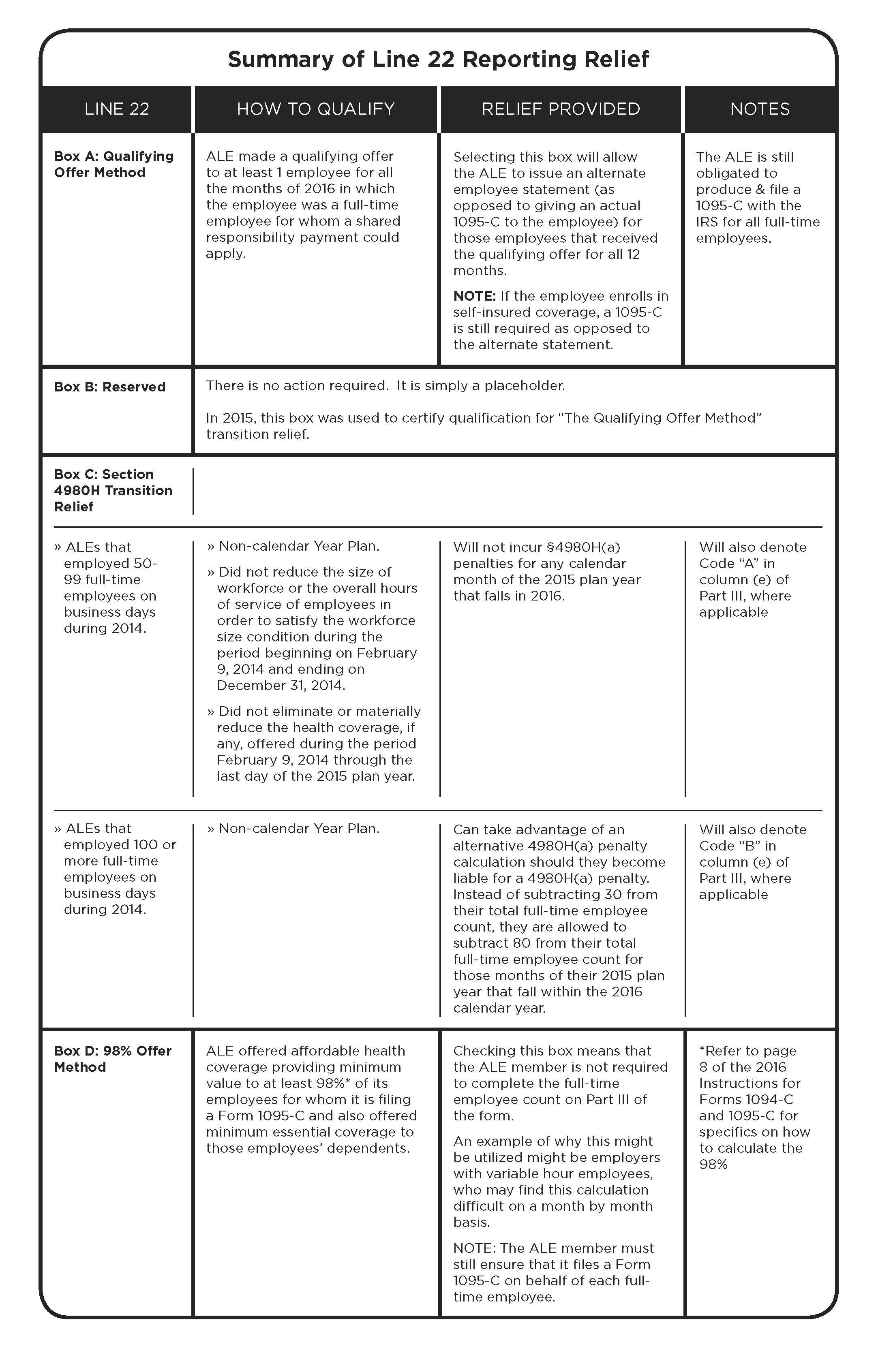
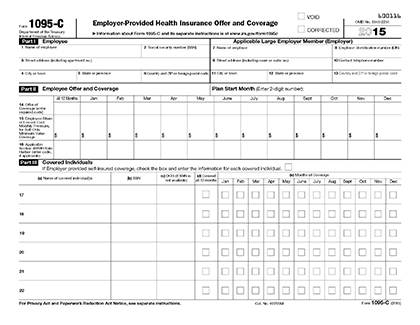
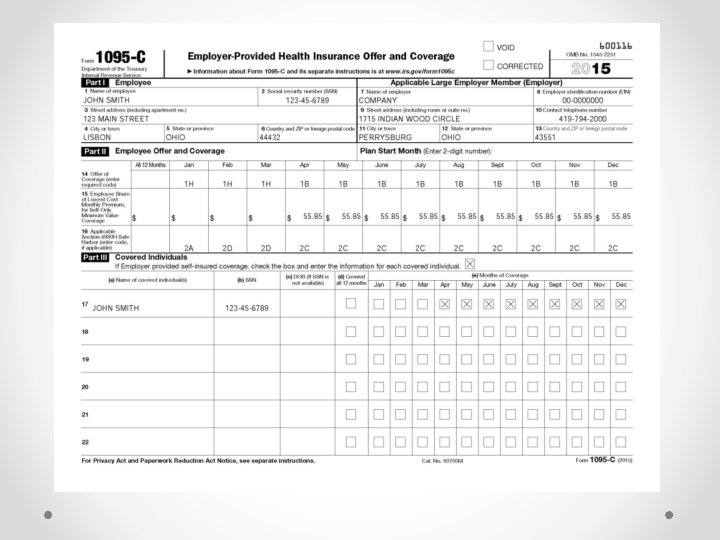
Jan 21, 16 · NC Department of Health and Human Services 01 Mail Service Center Raleigh, NC Customer Service Center For COVID19 questions call 1September 23, 1217 Line 14 on the 1095C is for the offer of coverage Enter the appropriate code in the All 12 Months box if the same code applies to the entire calendar year Or, if the offer of coverage changed during the year, enter the appropriate code in each of the individual monthlyFeb 09, 15 · Fulltime employees captured by slides 122 and 124 are the employees that the employer completed "1A" for on Form 1095C A 1A fulltime employee gets a substitute statement instead of Form 1095C under Line 22A so long as that 1A applies to all the months where the fulltime employee was a fulltime employee 125 126
An employee must receive a 1095C form whether or not they make use of the employer's health plan Where the 1094C Fits In While Form 1095C is sent to both employees and the IRS, Form 1094C is only provided to the IRS The following information must be included on Form 1094CFeb 24, · When populating Form 1095C, employers are communicating a lot of information through a series of codes on Lines 14 and 16 It is incredibly important for an employer to have documentation supporting the codes they are using when populating the Forms 1095C Below is a general breakdown of the different codes that could be entered on Lines 14You may receive multiple Forms 1095C if you worked for multiple applicable large employers in the previous calendar year You may need to submit information from the form(s) as a part of your personal tax filing Your employer generally is required to distribute your Form 1095C by January 31st, covering information for the previous calendar year
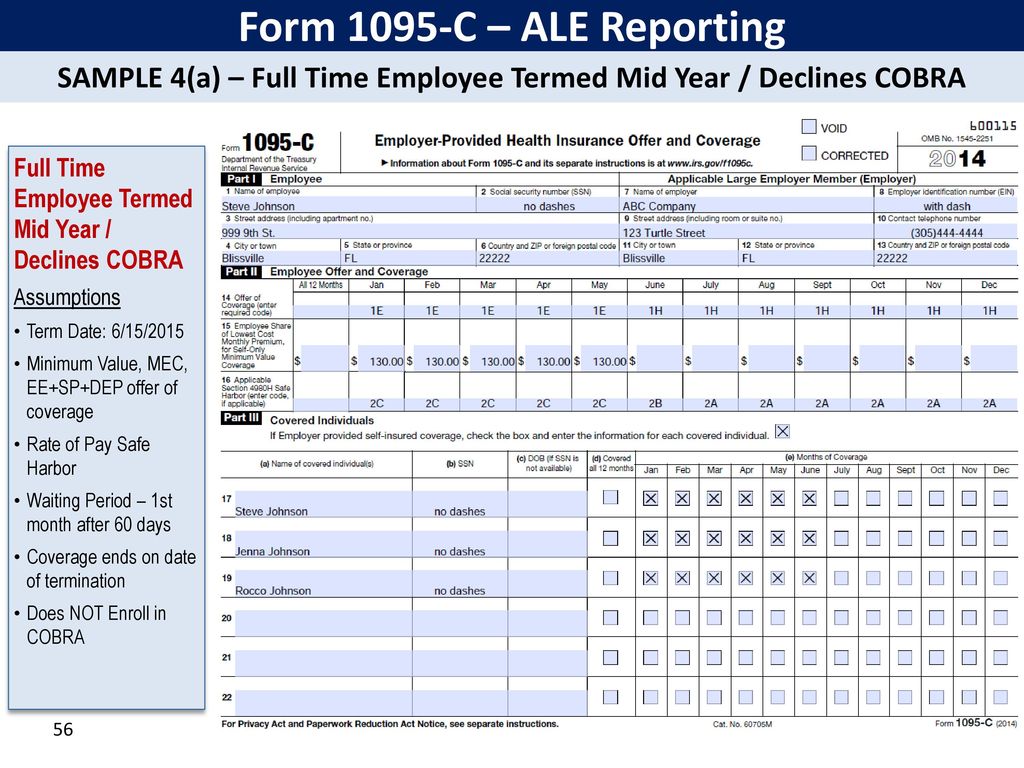


Irs Affordable Care Act Reporting Forms 1094 Ppt Download
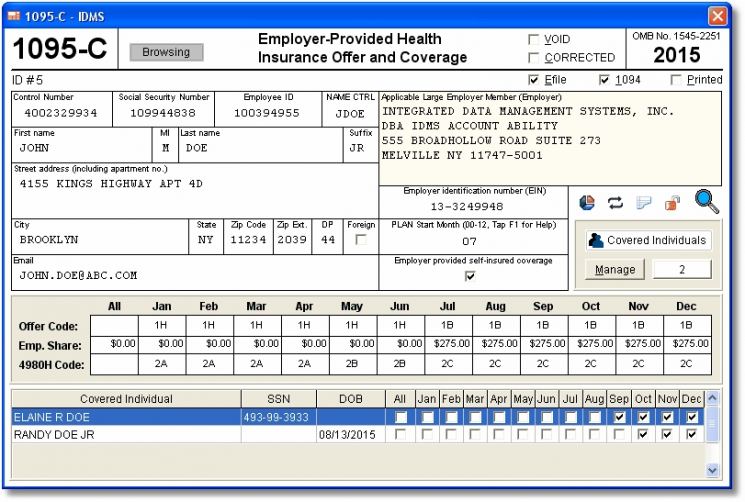


Account Ability S Aca 1095 B 1095 C Compliance Software Has Been Released Integrated Data Management Systems Inc Prlog
Feb 10, 16 · An employee who was in a limited nonassessment period for all 12 months of the year (for example, a new variable hour employee still in an initial measurement period) See the definition of Limited NonAssessment Period in the instructions to Form 1095C for more detailsOct 19, · For example, if an employee is offered coverage for plans that begin in January and July, the employee's Form 1095C plan start month box should be completed with 01 If there is no plan under which coverage is offered to the employee, 00 should be entered inOct , · Every ALE needs to provide a Form 1095C with Lines 1416 completed with the correct information Here is a breakdown of each line and what the corresponding codes mean Line 14 – Offer of Coverage
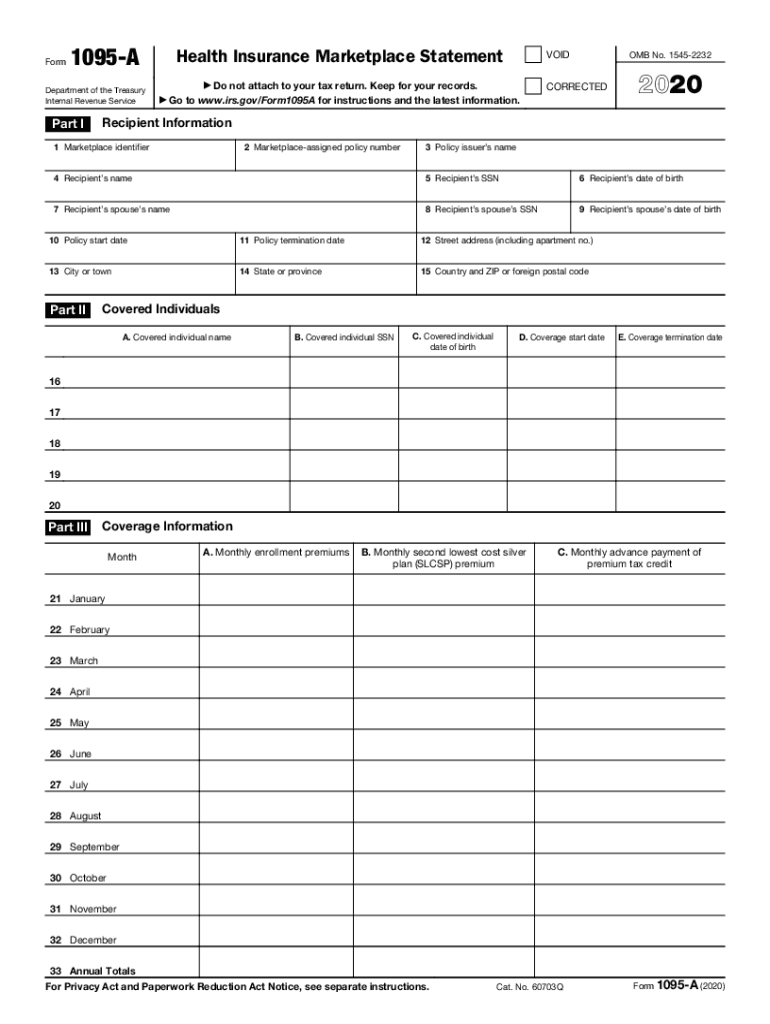


Form Irs 1095 A Fill Online Printable Fillable Blank Pdffiller


Aca 1095 C Basic Concepts
What is Form 1095C?Lockton Comment Examples include covered parttime employees, partners, nonemployee directors, independent contractors, retirees, and persons purchasing COBRA coverage Insert Code 1G in the "All 12 Months" box of line 14 Do not complete lines 15 and 16, but complete Parts I and III of the 1095CTwo minute tax topics – specific to the new form 1040 for 18 (filing in 19)https//wwwirsgov/pub/irspdf/i1040gipdfhttps//wwwirsgov/pub/irspdf/f1


Common 1095 C Coverage Scenarios With Examples Boomtax



Application Prototyping In Excel 1095 C Beyond Excel
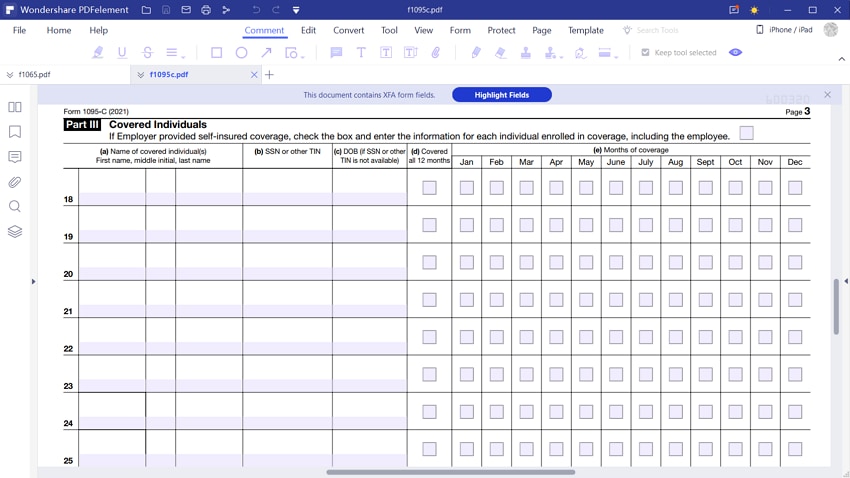
Oct 03, 18 · Self‐insured employers must report offers of COBRA coverage Employers complete Form 1095‐C providing COBRA coverage information (enrollment in COBRA coverage) How the Form 1095‐C is completed will depend, in part, on whether the employee was covered as an active employee during 18You should complete Part III of 1095C ONLY if the employer offers employersponsored selfinsured health coverage in which the employee or other individual enrolled For this purpose, employersponsored selfinsured health coverage does not include coverage under a multiemployer plan So you would not need to fill out this part of the formFeb 02, 16 · Yes, Form 1095C is required to be completed in the year that an employee terminates When employment termination is the COBRAqualifying event, COBRA is never reported as an offer of coverage – even if the former employee actually enrolls in COBRA coverage



Sample 1095 C Forms Aca Track Support



Aca Reporting Faq
The deadlines for filing Form 1095C with the IRS and furnishing copies to the recipient are as follows March 2, 21, is the deadline to distribute recipient copies March 1, 21, is the deadline to paper file Forms 1095C with the IRS March 31, 21, isMay 05, · Common 1095C Coverage Scenarios with Examples Completing 1095C forms can be confusing, but we're here to make it simple with this list of common 1095C coverage scenarios and examples As always, we are available to answer any questions you may haveForm 1095C is intended to include all the necessary information to allow the recipient and/or the tax preparer to properly complete and file the recipient's tax return All applicable large group employers (ALE's) are required to prepare, distribute and file IRS Form 1095C This form includes information that will


Common 1095 C Coverage Scenarios With Examples Boomtax
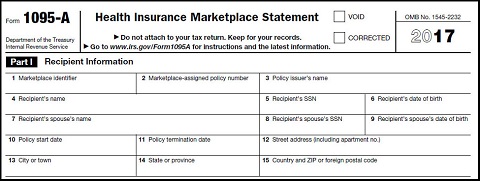


Form 1095 A 1095 B 1095 C And Instructions
Note that substitute forms may be used, but the substitute forms must include all of the information required by Forms 1094C and 1095C and must satisfy all of the IRS's form and content requirements Forms 1094B and 1095B are to be used by a small selfinsured employer that is not an ALE for Section 6055 purposesApplicable Large Employers (for example, you left employment with one Applicable Large Employer and began a new position of employment with another Applicable Large Employer) In that situation, each Form 1095C would have information only about the health insurance coverage offered to you by the employer identified on the formNov 30, · continues to create numerous hurdles and difficulties for employers One challenge for many employers, one that will carry into 21, is how to complete the required Forms 1094C and 1095C reporting for This overview outlines some of the common reporting situations employers face due to employee terminations and furloughs Many variables can


Common 1095 C Coverage Scenarios With Examples Boomtax



Aca Code Cheatsheet
Oct 02, 19 · To help employer complete forms 1094C and 1095C correctly, the IRS has provided answers to common questions These answers include instructions for reporting offers of COBRA continuation coverage The reporting requirements differ depending on whether COBRA was offered after termination of employment or after a reduction in hoursForm 1095C is a new form designed by the IRS to collect information about applicable large employers and the group health coverage, if any, they offer to their fulltime employees Employers will provide Form 1095C (employee statement) to employees and file copies, along with Form 1094C (transmittal form), to the IRSComplete lines 1 through 9 with current year Net Operating Loss (NOL) information Go to the section Computation of Decrease in Tax Enter the "Before Carryback" column of Lines 11 through 27, using the original tax returns from the carryback years as a reference



Irs Form 1095 C Codes Explained Integrity Data
:max_bytes(150000):strip_icc()/1095b-741f9631132347ab8f1d83647278c783.jpg)


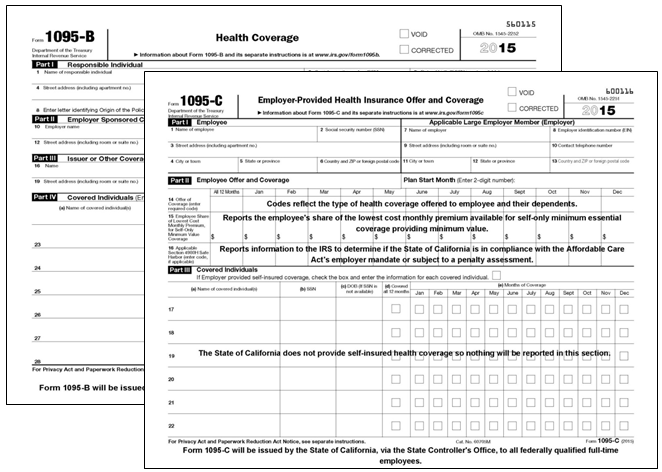
Form 1095 B Health Coverage Definition
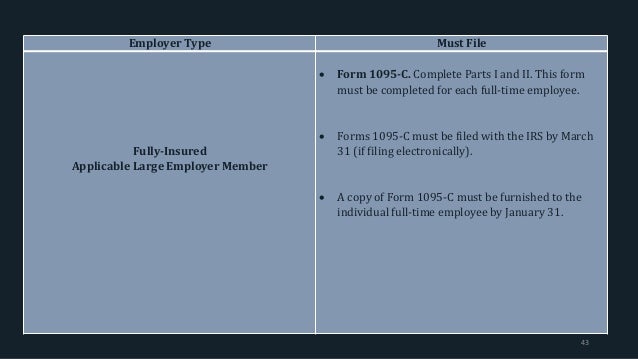
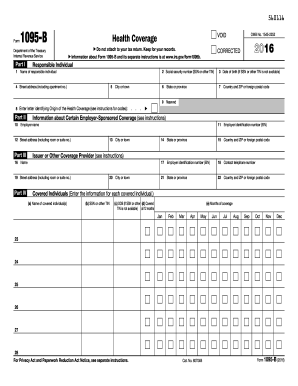
Aug 31, 15 · Specifically, part II of form 1095C is used to accomplish this task So yes your employees will need be receiving TWO 1095s 1095B will be issued by your carrier showing coverage on a monthbymonth basis Another 1095 will need to be completed by you the employer (1095C) with part I & II completed These forms are due at the same time asTo prove that they meet these requirements, companies need to file the Form 1094C and Form 1095C Filing season can be an administrative headache The IRS estimates that the Form 1094C alone can take up to four hours to complete The Form 1095C, which is sent to both employees and the IRS, clocks in at only 12 minutes per form For aFeb 03, 15 · Fully complete only Parts I and III for each nonfulltime employee covered under the selfinsured plan (and only complete Line 14 of Part II) Forms 1095C must be filed with the IRS by March 31 (if filing electronically) A copy of Form 1095C must be furnished to the individual fulltime employee by January 31


Common 1095 C Coverage Scenarios With Examples Boomtax


Irs Form 1095 C Fauquier County Va
May 04, 15 · Failure to understand those rules could lead to an accuracyrelated penalty for failure to correctly complete Form 1095C and/or assessment of a penalty under Internal Revenue Code Section 4980H In Part III, an employer who offers selfinsured health coverage must report the months during which an individual and each dependent was enrolled inMar 12, 15 · Here are a few more questions from our webinar, "Mastering 1095C Forms for ACA Compliance" If you missed the webinar, you can replay it hereThese questions cover measurement and stability periods, Union questions, waiting periods, and specifics on the formsSep 30, 18 · In March, you will receive your 1095C form The form can also be used to complete a person's tax return He recalled that an FTA member should only be interested 1 type of health form is a health tax Next calendar year, you may need to complete both your personal tax return 1095c information to prepare the tax return



Let S Look At The Most Common 1095 C Coverage Scenarios Integrity Data


Form 1095 C Guide For Employees Contact Us
Apr 14, 16 · If the Form 1095C has been filed with the IRS, a new, fullycompleted Form 1095C with the correct information must be submitted An "X" entered in the CORRECTED checkbox on the form The Form 1094C transmittal (not marked corrected) with the corrected 1095C forms must be filed with the IRS, and the employee must receive a copy of theJohn Barlament walks through how to fill out IRS forms 1094C and 1095C This presentation was given to selffunded employers at an Alliance Learning CircleSeries 1 and Code Series 2 in lines 14 and 16 of Form 1095C The IRS will then review the codes used and determine whether you are compliant with your employer mandate ACA requirements ACA FORM 1095C CODE SERIES The IRS has designed two sets of ACA codes to provide employers with a way to describe health coverage offers on Form 1095C



Sample Print Of 1095 B And 1095 C 1095 Software



1094 B 1095 B Software 599 1095 B Software
Mar 23, 16 · According to the IRS instructions for Forms 1094C and 1095C, if two or more employees employed by the same employer are spouses or employee and dependent, and one employee enrolled in a coverage option under the plan that also covered the other employee(s) (for example, one employee spouse enrolled in family coverage that provided coverage to the otherSep 23, · How do I complete line 14 on the 1095C form?Members of the Trust should not complete Part III of Form 1095C or check the box at the top of Part III FILLINGOUT FORM 1095C PART II FOR ACA FULLTIME EMPLOYEES Plan Start Month – This box is optional for 16 If you wish to complete it, enter the twodigit number (01 through 12) for the calendar month during which your plan year begins



Irs Form 1095 C Codes Explained Integrity Data


Irs Form 1095 C The Best Way To Fill It Out
Dec 14, 15 · With the Affordable Care Act comes the necessary paperwork that the IRS has to collect Doing so ensures that employers are providing a sufficient option of healthcare for its employees We've covered the Form 1095C, which is meant to lay out the offered insurance to each individual employeeThe 1094C must be filed with the Form 1095C, but it acts as a sort ofSep 23, · Line 15 on the 1095C is for the employee required contribution Line 15 is only required if you entered code 1B, 1C, 1D, 1E, 1J, 1K, 1L, 1M, 1N, 1O, 1P, 1Q, 1T, 1U on line 14 To complete line 15Once the form is completed, push Completed Distribute the completely ready form through email or fax, print it out or save on the equipment PDF editor permits you to make improvements in your Form 1095C from any online linked equipment, customise it as per your requirements, signal it electronically and distribute in various approaches



Aca And The Vista Hrms Fall Update


Health Services Tax Conference Day Two


Payroll Aca Reporting Rda Systems



Let S Look At The Most Common 1095 C Coverage Scenarios Integrity Data
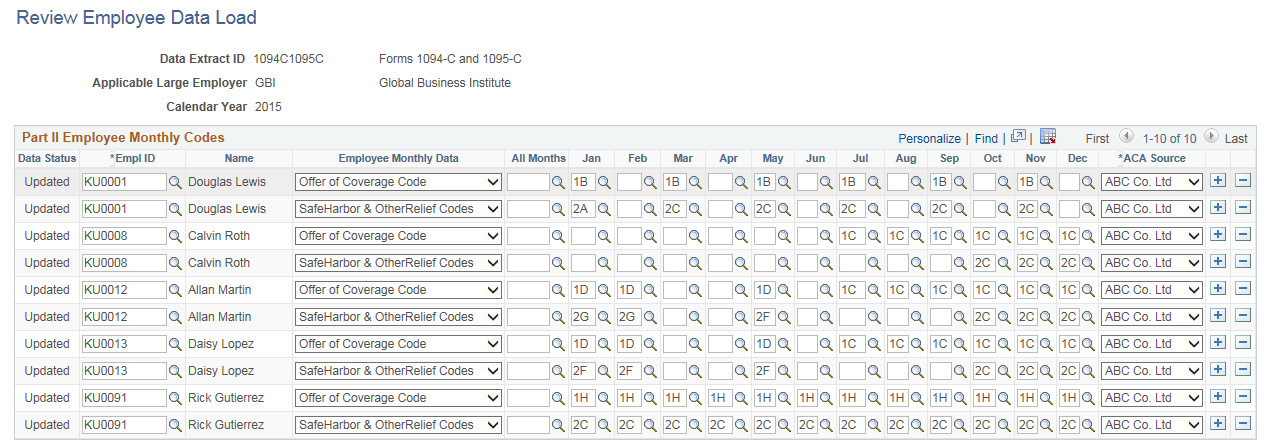


Creating Aca Form Data For Forms 1094 C And 1095 C



15 1095 Tax Form 1095 A 1095 B And 1095 C Tax Filing Obamacare Net



Aca Reporting Tip 19 Self Funded Plans Usi Insurance Services



Let S Look At The Most Common 1095 C Coverage Scenarios Integrity Data
/ScreenShot2021-02-08at3.59.40PM-9f028cea3cb545d19e4c64e10ca68a06.png)


Form 62 Premium Tax Credit Definition


Common 1095 C Coverage Scenarios With Examples Boomtax


United Benefit Advisors Home News Article



Explanation Of 2d On Line 16 Of The Irs 1095 C Form Integrity Data



Code Series 2 For Form 1095 C Line 16



1095 C Eemployers Solutions Inc



1095 C Faqs Office Of The Comptroller



Accurate 1095 C Forms A Primer Erp Software Blog


An Introduction To The Irs Aca Reporting Forms For Employer Reporting


Common 1095 C Coverage Scenarios With Examples Boomtax


Obamacare Tax Forms In The Time Of Coronavirus Don T Mess With Taxes


Aca 1095 C Basic Concepts



What Payroll Information Prints On Form 1095 C To Employees



Code Series 1 For Form 1095 C Line 14


1095 C Print Mail s



Affordable Care Act Aca Ability To Generate 1095 B And 1095 C Forms Microsoft Dynamics Ax Community



Ez1095 Software How To Print Form 1095 C And 1094 C


Sample Of 1095 C



15 1095 Tax Form 1095 A 1095 B And 1095 C Tax Filing Obamacare Net



1094 C 1095 C Software 599 1095 C Software


New Tax Document For Employees Duke Today



A Z Important Terms To Know For Forms 1094 1095 C Ts1099 Ts1099


Tom Mc Donald Presentation For 17 Aca July



Aca Code 1a Alert Irs Clarifies 1095 C Guidance For A Qualifying Offer Integrity Data



Sample 1095 C Forms Aca Track Support



Aca Reporting Tip 19 Self Funded Plans Usi Insurance Services



Aca Codes A 1095 Cheat Sheet You Re Gonna Love Thread Hcm



Let S Look At The Most Common 1095 C Coverage Scenarios Integrity Data



Irs Form 1095 C Codes Explained Integrity Data


Form 1095 A 1095 B 1095 C And Instructions


Common 1095 C Coverage Scenarios With Examples Boomtax



Aca And The Vista Hrms Fall Update



Aca Reporting Tip 16 Line 16 Union Employees Usi Insurance Services


Irs Form 1095 C The Best Way To Fill It Out



Ez1095 Software How To Print Form 1095 C And 1094 C



Sample 1095 C Forms Aca Track Support


F O R M 1 0 9 5 C E X A M P L E S Zonealarm Results



Common 1095 C Coverage Scenarios With Examples Boomtax



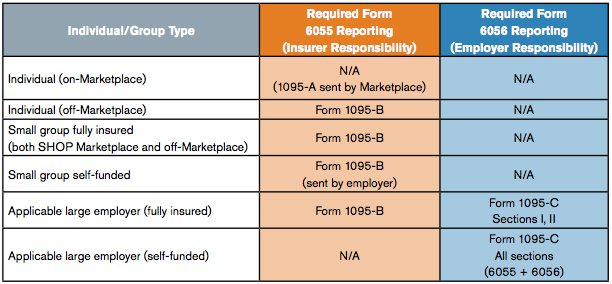
Aca Section 6055 And 6056 Health Coverage Reporting Ppt Download


Common 1095 C Coverage Scenarios With Examples Boomtax


The Affordable Care Act Upcoming Reporting Requirements October


An Introduction To The Irs Aca Reporting Forms For Employer Reporting
/ScreenShot2021-02-11at3.31.52PM-d4cdbd3f5e984eebb91c2b0478e46dc2.png)


Form 1095 C Employer Provided Health Insurance Offer And Coverage Definition



1094 C 1095 C Software 599 1095 C Software
:max_bytes(150000):strip_icc()/ScreenShot2021-02-11at3.31.52PM-d4cdbd3f5e984eebb91c2b0478e46dc2.png)


Form 1095 C Employer Provided Health Insurance Offer And Coverage Definition



Aca Reporting For Just Got More Complicated Syncstream Solutions


1095 C Submit Your 1095 C Form Onlinefiletaxes Com


Form 1095 A 1095 B 1095 C And Instructions


Overview Of 1095c Form
.png)


What Payroll Information Prints On Form 1095 C To Employees


Form 1099 Nec For Nonemployee Compensation H R Block


Annual Health Care Coverage Statements


1095 C Faqs Mass Gov



Let S Look At The Most Common 1095 C Coverage Scenarios Integrity Data


1095 C Reporting Requirements A Step By Step Guide



Irs Form 1095 C Codes Explained Integrity Data


Fillable 1095c Fill Online Printable Fillable Blank Pdffiller



0 件のコメント:
コメントを投稿